After epic debate, avian flu research sees light of day
After a marathon debate over a pair of studies that show how the avian H5N1 influenza virus could become transmissible in mammals, and an unprecedented recommendation by a government review panel to block publication, one of the studies was finally and fully published today (May 3, 2012) in the journal Nature.
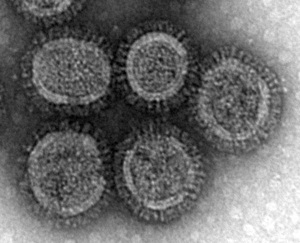
Pictured is a microscopic view of an unaltered, wild-type avian H5N1 virus. A study by researchers in the lab of Yoshihiro Kawaoka at the University of Wisconsin–Madison’s School of Veterinary Medicine shows that just a handful of mutations are required to make the H5N1 virus transmissible in mammals. The study demonstrates that circulating H5N1 virus, such as the ones pictured here, could pose a threat of pandemic flu should the mutations observed in laboratory studies occur in nature.
Photo: Dr. Takeshi Noda, University of Tokyo
Publication caps an epic public conversation that pitted some infectious diseases experts against flu and public health researchers who argued that publication was not only important, but also essential to informing influenza surveillance and preparedness for a virus that could evolve to infect humans and cause a global pandemic.
“Our study shows that relatively few amino acid mutations are sufficient for a virus with an avian H5 hemagglutinin to acquire the ability to transmit in mammals,” says Yoshihiro Kawaoka, a University of Wisconsin–Madison flu researcher whose study of H5N1 virus transmissibility was at the center of the debate. “This study has significant public health benefits and contributes to our understanding of this important pathogen. By identifying mutations that facilitate transmission among mammals, those whose job it is to monitor viruses circulating in nature can look for these mutations so measures can be taken to effectively protect human health.”
However, Kawaoka cautions there may be other unknown mutations that also enable the virus to transmit in mammals. It is therefore critical, he argues, to continue research to identify additional mutations that have the same effect, and to understand how they work.
The study, conducted by an international team of researchers led by Kawaoka, a UW–Madison professor of pathobiological sciences and a leading expert on influenza, shows that some viruses now circulating in nature require just four mutations to the hemagglutinin protein, which sits on the virus surface and enables it to bind to host cells, to become an even greater threat to human health. A subset of the mutations identified by the Wisconsin group has, in fact, already been detected in some viruses circulating in poultry flocks in Egypt and parts of Southeast Asia, underscoring the urgency of science-based surveillance, Kawaoka says.
In the Nature report, Kawaoka’s group describes a laboratory-modified bird flu/human flu hybrid virus that can become transmissible in an animal model for human infection with just a handful of mutations. Because flu viruses in nature are constantly changing as they circulate and easily swap genes with other flu viruses, the possibility of circulating H5N1 viruses hitting the right combination of mutations and becoming a much bigger threat to human health is greater than many experts believed, avers Kawaoka, a faculty member in the UW–Madison School of Veterinary Medicine.
“H5N1 viruses remain a significant threat for humans as a potential pandemic flu strain. We have found that relatively few mutations enable this virus to transmit in mammals. These same mutations have the potential to occur in nature,” explains Kawaoka.
Since late 2003, the H5N1 viruses have infected at least 600 humans, mostly in Asia, and killed more than half of the people infected. But the virus, which can be acquired through close contact with domestic fowl, does not easily transmit from human-to-human, a phenomenon that led some scientists to believe H5N1 posed little threat as a potential agent for a global flu pandemic. However, research on transmission of viruses from animal reservoirs was deemed a priority by the United States National Institute of Allergy and Infectious Disease (NIAID) in a 2006 Blue Ribbon Panel report, as well as by the World Health Organization (WHO) in its 2009 Public Health Research Agenda.
In addition to demonstrating transmissibility, Kawaoka’s results showed the experimental mutant virus could be controlled by available medical countermeasures. An H5N1 vaccine as well as oseltamivir, an antiviral drug better known by the trade name Tamiflu, both proved effective.
The study was conducted with scientists from the University of Tokyo, where Kawaoka is also on the faculty, Kobe University, and Chubu University.
The flu virus depends on an ability to enter and commandeer host cells to make new virus particles, which go on to infect other cells and spread to other hosts. But flu virus, which typically arises in animal reservoirs such as domestic fowl and pigs before spreading to humans, must adapt by changing its surface topography to match those of a new host species. A protein on the surface of the virus known as hemagglutinin is one of the keys that allow the virus to access host cells. It utilizes a bulb-shaped structure called the “globular head” to bind to host cells at the time of infection. The amino acids in this portion of the hemagglutinin protein are like a combination that opens a locked cell. Without the right combination, the virus is unable to enter a host cell and cause infection.
But flu viruses are masters of shape shifting, a characteristic that helps them adapt to new animal hosts. They readily exchange genetic information and mutate to acquire the molecular features that can make them more infectious.
Whether or not the H5N1 viruses currently circulating in the world can easily acquire the additional mutations needed to cause a pandemic is an open question, according to Kawaoka: “It is hard to predict. The additional mutations may emerge as the virus continues to circulate.”
The new work will aid those who monitor flu and could provide a critical early warning. “Should surveillance activities identify flu strains accumulating additional key mutations, these emerging viruses should then be priority candidates for vaccine development and antiviral evaluation,” says Kawaoka.
One important upshot of the study by Kawaoka’s group is the identification of the mechanism by which the H5N1 virus transmits, a basic discovery that could aid in the development of countermeasures, and that contributes to the store of basic knowledge on influenza virus transmission.
The work will also help governments in some countries justify the significant economic hardship imposed by the mass culling of poultry flocks when potentially dangerous mutations are identified in circulating H5N1 viruses.
The new study was conducted using ferrets, a widely accepted model for influenza research because, when infected with the flu virus, they sneeze and cough, generating small droplets that can carry the virus from one animal to another, demonstrating transmissibility. The ferret respiratory tract also has cellular features similar to those found in humans.
In December 2011, a National Institutes of Health advisory panel, the National Science Advisory Board for Biosecurity (NSABB), recommended redacting critical information from the Kawaoka lab’s report, as well as from a similar study conducted in Holland. The unprecedented request was to withhold the methodologies used to make the virus transmissible and to not identify the mutations needed to make the virus transmissible in mammals. This month, the NSABB reversed itself, citing new information and manuscript revisions that more explicitly state the public health rationale for the work as well as the safety and security precautions in place in the labs in Wisconsin and Holland.
It was noted that the virus engineered in Kawaoka’s lab was, in fact, of low virulence. The hybrid virus was made by building the H5N1 hemagglutinin gene into the pandemic H1N1 flu virus; the H5-H1N1 hybrid was less pathogenic than pandemic H1N1 virus.
As is the case for all studies of avian influenza transmissibility, the Wisconsin H5N1 work was conducted under strictly controlled conditions with multiple layers of safety and security precautions. Moreover, research involving agents such as highly pathogenic influenza viruses undergoes rigorous federal and institutional oversight including frequent and unannounced inspections. The laboratories such as the one where the new work was conducted are designed to strict specifications and operated to ensure safety.
The animal study of virus infectivity was supported by NIAID, a part of the National Institutes of Health. Other elements of the new study were supported by the Bill & Melinda Gates Foundation, by a Grant-in-Aid for Specially Promoted Research from the Ministry of Education, Culture, Sports, Science, and Technology of Japan and by ERATO, the Japan Science and Technology Agency.
Tags: federal relations, influenza, research




